Diabetes
Last Modified 17/02/2025 15:19:04
Share this page
Introduction
Diabetes is a life-long metabolic disease characterised by elevated levels of blood glucose (blood sugar). With diabetes the person is unable to adequately produce or regulate their insulin, resulting in erratic blood glucose levels, lipid levels and the potential for renal and liver damage, as well as serious damage to the heart, blood vessels, eyes, and nerves. It is a major health concern as local and national rates are expected to increase.
There are two main types of diabetes: type 1 is an autoimmune condition resulting in 'insulin dependence' as the person's pancreas fails to produce any insulin to control blood glucose levels, and therefore requires insulin injections for life. Type 2 is known as 'insulin resistant' and is the more common type of diabetes, accounting for 90% of adults with diabetes.1 Type 2 is a progressive disease, but often in the earlier stages can be controlled by eating a healthy diet, maintaining a healthy weight, and exercise.
Long-term conditions in children provides information on childhood diabetes (type 1) in Blackpool.
Facts and figures
Prevalence of diabetes
For further information regarding the source of NHS Quality and Outcomes Framework (QOF) prevalence data and its limitations please see the note on QOF Data.
In 2023/24, 13,699 people aged 17 and over in the Blackpool ICB sub-location (formerly NHS Blackpool CCG) were identified as living with diabetes. This equates to 9.3%, which is significantly higher than the England average (7.7%) and has been rising year on year from 6.9% in 2012/13.2
Blackpool's sub-location is shown as a purple marker in figure 1, with all other sub-locations shown in blue. Blackpool's diabetes prevalence is the seventh highest rate in England.
It is important to highlight the risk of an impaired glucose state ('metabolic syndrome'), in which a person is not diabetic but their lifestyle leaves them at high risk of developing type 2 diabetes. Contributing lifestyle factors include unhealthy diet, excess weight and lack of exercise. If these lifestyle factors are changed, the onset of type 2 diabetes can be prevented.
Figure 1 - diabetes prevalence (17 and over) funnel plot analysis at sub-location level (2023/24 QOF)
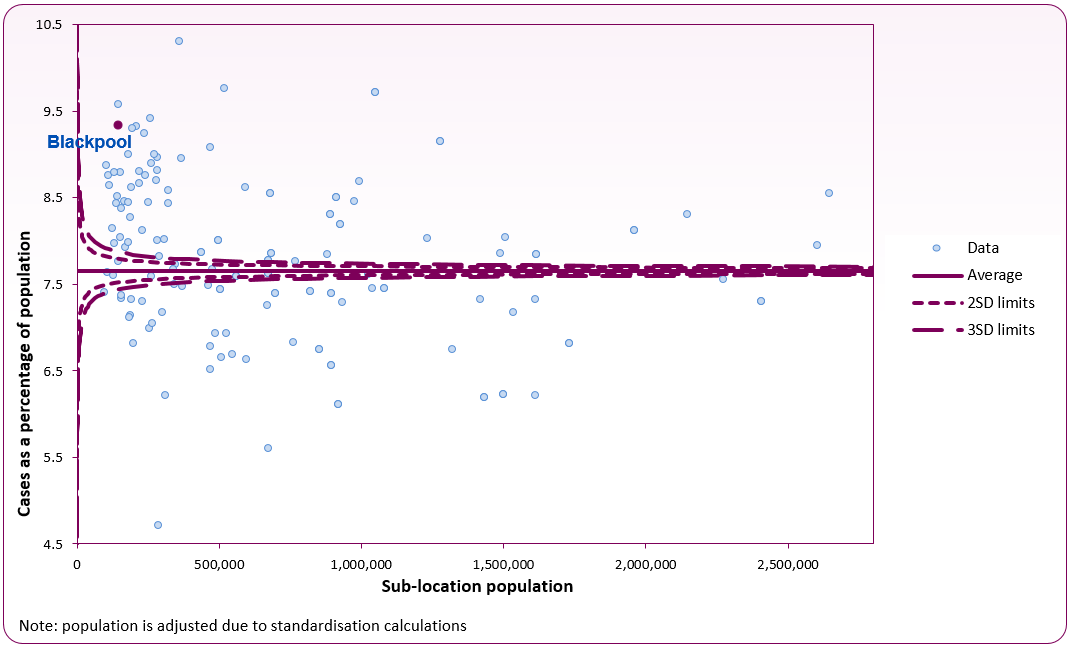 Source: Office for Health Improvement and Disparities Diabetes Profile
Source: Office for Health Improvement and Disparities Diabetes Profile
Figure 2 shows diabetes prevalence in all GP practices that make up Blackpool's sub-location (formerly NHS Blackpool CCG). There is a considerable range in recorded prevalence of diabetes from 7.0% to 10.3%. Four of the GP practices (yellow) are significantly similar to England's prevalence (7.7%) - Arnold Medical Centre, Marton Medical Centre, Newton Drive Health Centre and South King Street Medical Practice. The remaining 12 are significantly higher.
Figure 2 - diabetes prevalence (17+) funnel plot analysis at GP level (2023/24 QOF)
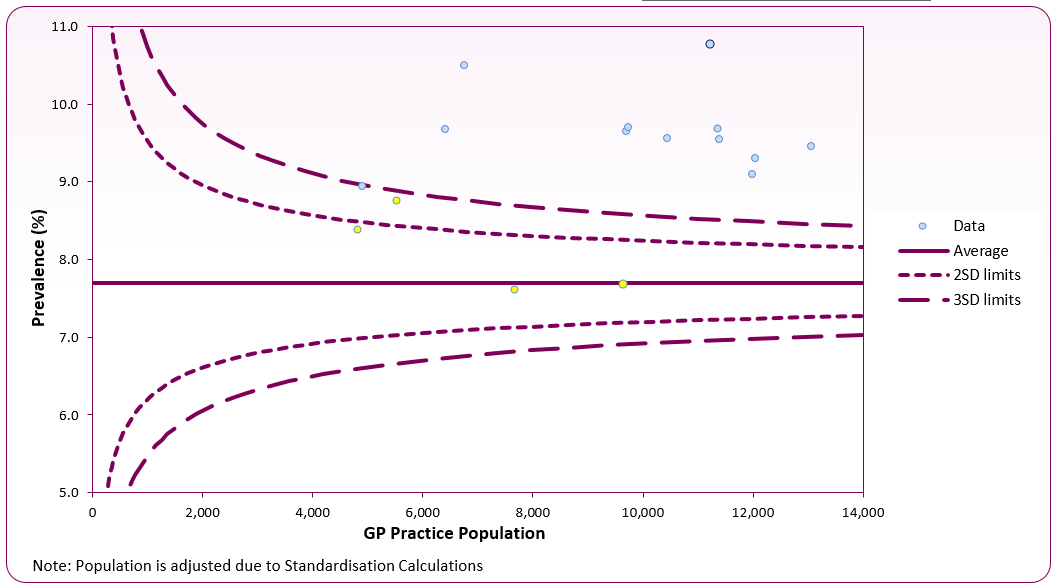 Source: OHID Diabetes Profile
Source: OHID Diabetes Profile
National Diabetes Audit (NDA)
The National Diabetes Audit (NDA) provides a comprehensive view of diabetes care in England and Wales, measuring the effectiveness of diabetes healthcare across nine care measurements that people living with diabetes should expect to receive on an annual basis:
- Weight and body mass index (BMI)
- Blood pressure
- HbA1c (blood glucose level)
- Retinopathy screening
- Foot surveillance
- Urinary albumin test
- Serum creatinine
- Smoking status
- Cholesterol level
The findings from the 2023-24 NHS Digital Core NDA show that there were 875 registrations for type 1 diabetes in Blackpool and of these, 57% were male. For type 2, there were 12,605 registrations, with 58% male.
Looking at type 1 diabetes, 38.9% of Blackpool patients were recorded as having all nine care processes checked in 2023-24, compared to 42.2% nationally. Almost a half (47.4%) had eight care processes checked (excluding retinopathy) compared to 47.2% nationally. For type 2 diabetes, 51.2% of Blackpool patients were recorded as having all nine care processes checked compared to 54.3% nationally. Two-thirds (66.9%) had eight care processes checked (excluding retinopathy) compared to 62.4% nationally.
HbA1c is a person's average blood glucose (sugar) level. For those with diabetes, a standard target range of 48 mmol/mol or lower (6.5%) is desirable to lower the risk of long-term vascular complications, though this target may change depending upon age or other individual factors. In 2023 -24, 13.2% of those registered with type 1 and 32.0% of those with type 2 diabetes had a recorded HbA1c level at or below this. Levels are similar to the national average for those with type 1 and type 2 diabetes (figure 3).
Figure 3: percentage of patients with diabetes (types 1 & 2) with HbA1c <= 48 (6.5%), Blackpool and England, 2016/17 to 2023/24
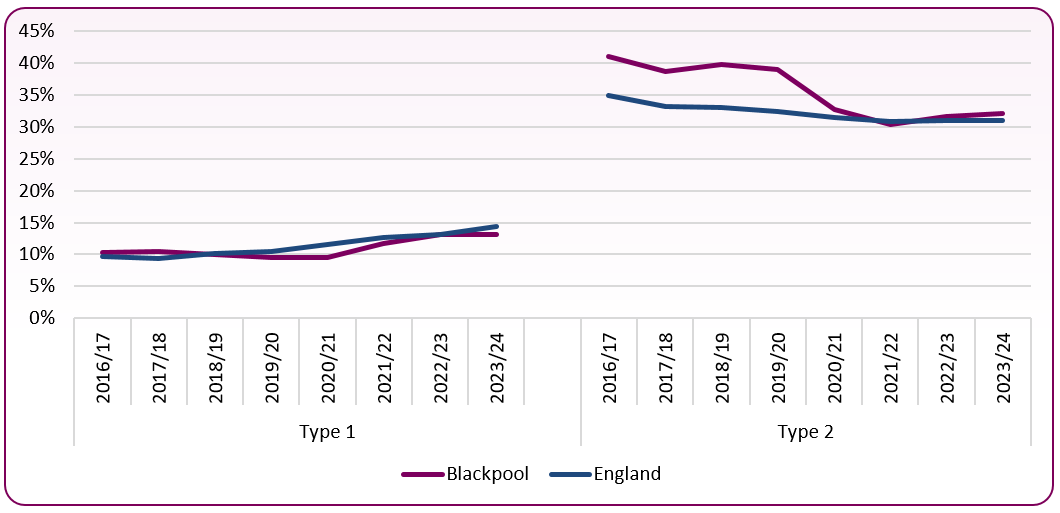 Source: NHS Digital National Diabetes Audit
Source: NHS Digital National Diabetes Audit
National and local strategies (current best practices)
-
- The National Service Framework for Diabetes (Department of Health, 2001) sets out 9 standards for the provision of high quality services, which include the identification, empowerment and care of patients with diabetes.
- The National Diabetes Audit sets out the '9 Key Care Processes' that form a planned programme of recommended checks that all patients with diabetes are expected to receive each year. Participation in the audit is voluntary, so not all GP practices participate.
- NICE guidance [PH38] Type 2 diabetes: prevention in people at high risk (updated September 2017) covers how to identify adults at high risk of type 2 diabetes. The 20 recommendations in this guideline can be used alongside the NHS Health Check programme.
- NICE guidance [PH35] Type 2 diabetes prevention: population and community-level interventions (May 2011) covers preventing type 2 diabetes in adult populations and communities who are at high risk. It aims to promote a healthy diet and physical activity at community and population level, and recommends how to tailor services for people in ethnic communities and other groups who are at particular risk of type 2 diabetes.
Risk factors
Risk factors associated with developing type 2 diabetes:
-
- being overweight or obese - having a waistline greater than 94 cm (37 inches) for men or greater than 90 cm (35 inches) for men of South Asian origin. For women, having a waistline greater than 80 cm (31.5 inches)
- aged 40-years and over, or for people of South Asian origin, 25-years and over
- having parents, or a brother or sister, with type 2 diabetes
- being of Black African, or Black Caribbean origin (three times more likely to develop type 2 diabetes) or South Asian origin (six times more likely to develop type 2 diabetes)
- being a woman who has had gestational diabetes or has had a baby weighing more than 4.5kg (9.9lbs) at birth
- being an overweight woman with a history of polycystic ovarian syndrome
- having a history of high blood pressure, heart attack or stroke
- having ever experienced higher than normal blood glucose levels - impaired glucose regulation (IGR) - also known as impaired glucose tolerance, impaired fasting glucose, non-diabetic hyperglycaemia or pre-diabetes
- having a mental health condition such as schizophrenia, bipolar illness or depression, or if someone is taking antipsychotic medication
Obesity is the most potent risk factor for type 2 diabetes. It accounts for 80-85% of the overall risk of developing type 2 diabetes. Almost two in every three people in the UK are overweight or obese.
Individuals with diabetes also have a higher risk of retinal damage (diabetic retinopathy). This is when high blood sugar levels cause blood vessels in the eye to become damaged. They may become blocked, have excess fluid or leak, causing blurred visions, and in worst case, blindness. The NHS Diabetic Eye Screening Programme is therefore essential for identifying retinopathy at an early stage. Every individual over the age of 12 with diabetes should be invited for a screening once a year.
[]Diabetes UK, State of the Nation 2012
[]Office for Health Improvement and Disparities (OHID), National General Practice Profiles